The COVID Hot Potato: Patients with non-COVID illnesses are suffering: healthcare professionals report the hospital capacity exists but we need the strategy now
Mon, 27 April 2020
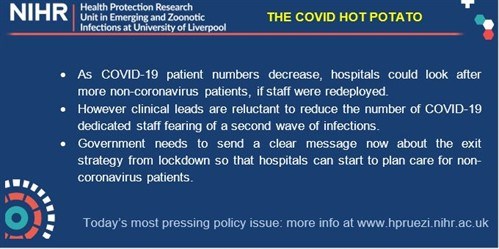
Emerging issue: Hospitals need a government lead on the lockdown exit strategy to plan the right mix of services as health needs change following the COVID-19 ‘peak’
OVERVIEW: Hospital staff rotas have been prepared based on anticipated demand of COVID-19 patients, but as the number of patients presenting plateaus or even reduces there are surplus clinical staff beyond what is needed. While this is seen as positive, previous fears on lack of capacity in hospitals present a new challenge when planning for staff needs as the response continues.
CONCERNS ABOUT INCREASED CAPACITY: These are exemplified by a junior doctor in London who has been redeployed from Obstetrics and Gynaecology to Medical Wards reported that they have found that there is not enough work for all staff to complete during a shift as COVID-19 patient numbers have decreased. While this is frustrating for staff that are being asked to work additional hours (and more weekends/nights), it is also causing anxiety in terms of being away from specialty training. Junior doctors in particular are concerned about how they will complete the required training that is necessary to progress in chosen specialties.
CONCERNS ABOUT REDUCING STAFF NUMBERS: A clinical lead in an Emergency Department in a District General Hospital, North Midlands, for example, reported that they are aware that changes to their rota currently mean that staff capacity may be greater than demand. However, they do not want to reduce the number of staff in case of a second wave of infection. Lack of communication about the length of time current lockdown measures are in place means that it is difficult to plan ahead, both in terms of staffing and communicating these plans to staff. They reported that their decision-making would be better facilitated by knowing what they were planning for.
THE NEED TO REINTRODUCE SERVICES: The number of non-COVID-19 patients presenting to Emergency Departments is increasing. The Clinical Lead in North Midlands and a registrar in Essex highlighted the need to consider how to redistribute resources in units that have been altered to ensure separate zones for COVID-19 and non-COVID-19 patients. These units need to be able to plan appropriately to ensure patients receive the best care.
REDEPLOYING & REPURPOSING STAFF: A pain specialist nurse redeployed to an ITU in a London hospital reported that staff may be waiting long periods to be redeployed, as there is a lack of communication about changes regarding what kind of staff are needed where. Reviewing changing demand in different hospitals needs to be better communicated to staff. A respiratory nurse redeployed to an intensive care unit in a London hospital reported that staff who are unable to care for COVID-19 patients (e.g. pregnant, underlying health conditions) are helping in hospital call centres to communicate with patient families, suggesting that surplus staff could be drawn upon in the short-term for different kinds of support.
CONCLUSION: Strategies must adapt promptly as health needs change. Hospitals cannot yet plan to accommodate increasing numbers of non-COVID-19 patients whilst COVID-19 patient numbers decrease. The government must communicate the anticipated length of peak demand and current lockdown measures to enable planning at Trust level.
NOTE: The NIHR Health Protection Research Unit in Emerging and Zoonotic Infections brings together internationally leading researchers from the University of Liverpool, University of Oxford, Liverpool School of Tropical Medicine, and Public Health England.
We are conducting an MRC/NIHR-Funded project to understand the dynamics of policy development and healthcare professionals’ behaviour in the UK during the COVID-19 pandemic. We have a targeted panel of healthcare professionals, with whom we regularly speak, to capture their experiences and reactions over the course of the outbreak. They include clinical leads, junior doctors, and nurses in high consequence infectious diseases (HCID) units, Emergency departments, intensive therapy units, medical wards, neonatal units and GP surgeries.
We have previously identified emerging issues around PPE challenges, the need for testing of healthcare professionals, and the need for mental health support for staff on the frontline, all of which were fed back to Government Advisory Panels, and proved to be important in decision-making.