The COVID Hot Potato 4
Thu, 14 May 2020
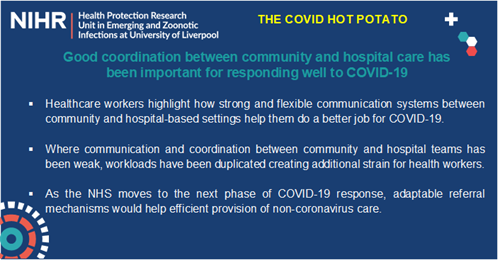
This week: Healthcare professionals reflect on health system resilience, with those in Scotland talking about how relationship-building within and between community and hospital teams has been important in responding well to COVID-19.
A GP in the Shetland Islands reflected on how community and hospital healthcare teams have worked together: “Speaking from the community side of things, it’s gone quite well. We’ve just had to do it, there’s no extra GPs we could call on to run the COVID assessment hub, and it is run by GPs not the hospital… I’ve enjoyed the ways we’ve therefore had to link in with the hospital and I think improved relationships between hospital and community, and that goes a long way. I think we’ve managed well.”
Earlier in the response, she described how workloads were being duplicated due to poor coordination and communication, leading to frustration and inefficient working: “Chains of command are different for each team of people. Hospital specialists, and then GPs, and then nurses in community all have really different management...what we’re finding is that [nurses] are being asked to do a lot of stuff that actually I’ve already done…and it’s all just happening independently and at odds, sometimes, with what we’re doing.”
Comparatively, a registrar in an Emergency Department in England highlights how existing mechanisms are not well-suited to the current crisis for referring and discharging patients between community and hospital care, especially as A&E will potentially see more chronic health issues and possible cancer diagnoses as the country comes out of lockdown and the NHS transitions to the next phase of the response. “As a GP, you can send a patient for further investigation to a clinic…I don’t have those systems in place in A&E. If I send someone to a clinic, the clinic then have to write back to the GP…they can’t write back to me, because I don’t coordinate their care, I coordinate their emergency care…the structure is not there.”
NOTE: The NIHR Health Protection Research Unit in Emerging and Zoonotic Infections brings together internationally leading researchers from the University of Liverpool, University of Oxford, Liverpool School of Tropical Medicine, and Public Health England.
We are conducting an MRC-Funded project to understand the dynamics of policy development and healthcare professionals’ behaviour in the UK during the COVID-19 pandemic. We have a targeted panel of healthcare professionals, with whom we regularly speak, to capture their experiences and reactions over the course of the outbreak. They include clinical leads, junior doctors, and nurses in HCID units, Emergency departments, intensive therapy units, medical wards, neonatal units and GP surgeries.
We have previously identified emerging issues around PPE challenges, the need for testing of healthcare professionals, and the need for mental health support for staff on the frontline, all of which were fed back to Government Advisory Panels, and proved to be important in decision-making.